Quality Resource Guide –
Oral Ulcerative and Vesiculobullous Diseases Part 1 - 4th Edition
www.metdental.com
Page 3
(>1.0 cm) and more painful and persist longer
than minor aphthae, typically six weeks or longer,
with a post-pubertal onset. Because of the depth,
extent and duration of inflammation, major
aphthous ulcers appear as a crater clinically and
typically heal with scar formation. Lesions may
take up to 6 weeks or longer to heal, and as soon
as one ulcer disappears, another one often starts.
In patients who experience an unremitting course
with significant pain and discomfort, systemic
health may be comprised because of difficulty in
eating and psychological stress. The predilection
for movable oral mucosa is typical for major
aphthous ulcers as it is for minor aphthae while
HIV-positive patients may have aphthous lesions
at any intraoral site.
Herpetiform Aphthous Ulcers
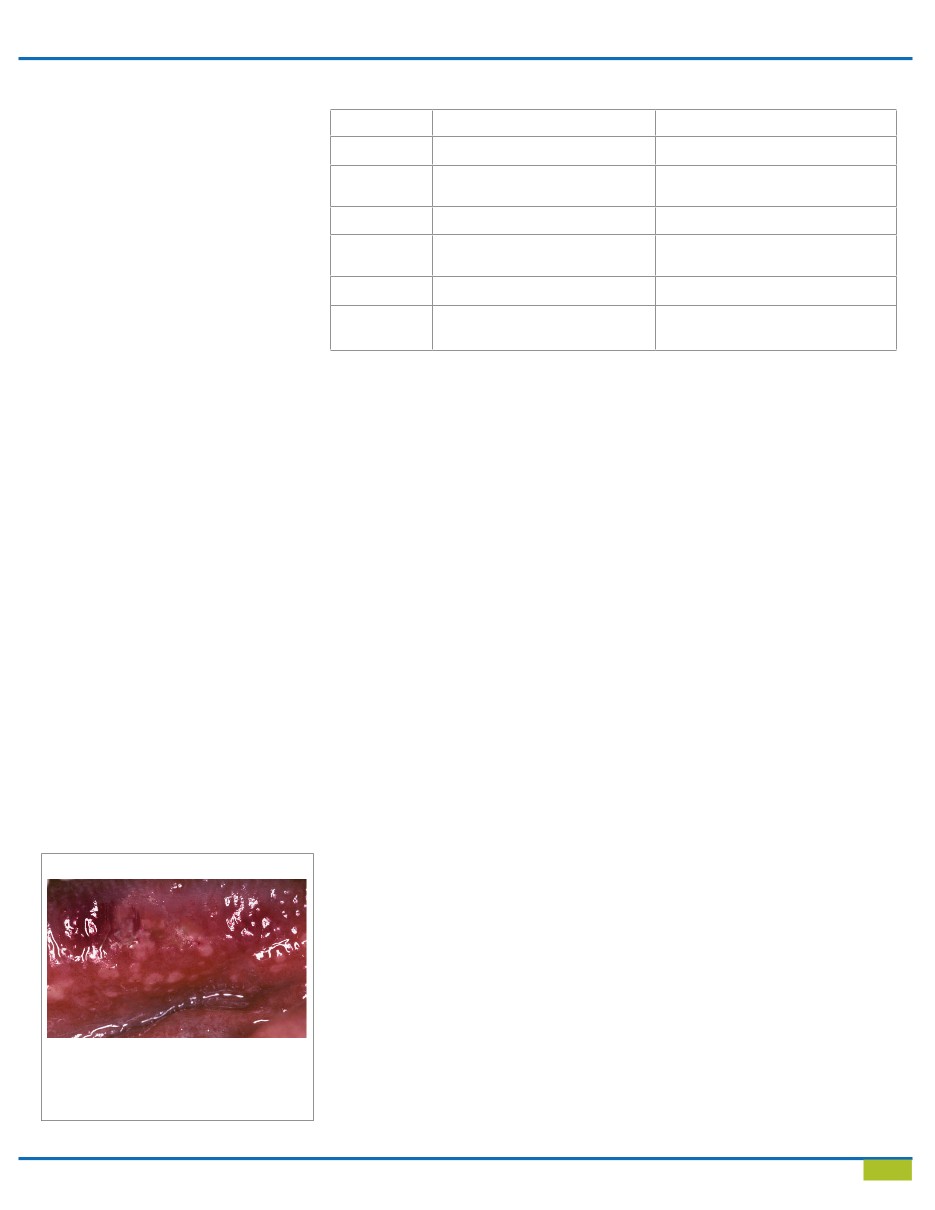
Herpetiform aphthous ulcers present clinically as
recurrent crops of small ulcers (Figure 4) and arise
in 1-10% of those with aphthous ulcers. Although
movable mucosa is predominantly affected,
palatal and gingival mucosa may also be involved,
often characterized by coalescence and formation
of larger, more irregular ulcers. Pain may be
considerable, and healing generally occurs in
1 to 2 weeks. Unlike herpes infections themselves,
herpetiform aphthous ulcers are not preceded by
vesicles (as a key distinguishing feature from
recurrent primary herpes simplex infections) and
exhibit no viral-infected cells. Other than the
clinical feature of crops of oral ulcers, there has
been no finding that can link this disease to a
viral infection.
Histopathology
Aphthous ulcers have nonspecific microscopic
findings, with no histologic features that are
diagnostic. Virus-infected cells are not evident.
Essentially, the same nonspecific microscopic
changes are found in all forms of aphthous
ulcers.
Differential Diagnosis
Diagnosis of aphthous ulcers is generally based on
history and clinical appearance. Lesions of secondary
(recurrent) oral herpes can mimic aphthous ulcers
but can usually be distinguished from them based on
history and physical examination (Table 2).
A history
of vesicles preceding ulcers, location on the attached
gingiva and hard palate, and crops of lesions indicate
herpetic rather than aphthous ulcers. Other painful
oral ulcerative conditions that may simulate the
various forms of aphthous ulcers include traumatic
ulcers, pemphigus vulgaris, mucous membrane
pemphigoid, enterovirus infections (hand, foot,
mouth disease) and neutropenia-related ulceration.
Treatment
In most patients with an occasional or a few
minor aphthous ulcers, no treatment is usually
indicated apart from a bland mouthrinse such as
sodium bicarbonate in warm water to keep the
mouth clean. Over the counter preparations such
as amlexanox may be effective. However, when
patients are more severely affected, other forms of
prescription level treatment can provide significant
control (but not necessarily a cure) of this disease.
Rational treatment would include drugs that can
manipulate or regulate immune and inflammatory
responses including corticosteroids (triamcinolone
acetonide, fluocinonide gel), diaminodiphenyl
sulfone
and others (Table 2). In this category
corticosteroids currently offer the best chance for
disease containment. In severely affected patients
systemic steroids may be used for immediate
control. A low to moderate dose of prednisone
for a short period is effective. A typical regimen
might be 20 to 40 mg. daily for one week,
followed by another week at half the initial dose
before discontinuation. However, for patients with
mild to moderate disease, topical mono-therapy
only, paired with topically placed lidocaine, is
usually effective. Topically applied steroids, if used
judiciously, can be relatively efficacious and safe.
Although nearly all topical steroid compounds
have been developed for use on skin, it has been
standard practice to prescribe these agents for use
on mucous membranes for limited periods of time.
Intralesional injection of triamcinolone may be used
for individual or focal problematic or recalcitrant
lesions.
Other Drugs
Recent studies indicate that thalidomide may
provide relief to severely affected patients,
especially AIDS patients. This drug is considered
to reduce TNF-alpha levels, inhibit neutrophil
chemotaxis, stabilize lysosomal membranes and
reduce local free radical formation, among other
properties. Two other drugs that have shown some
therapeutic efficacy at the systemic level for oral
ulcerations as a component of a complex aphthous
stomatitis are pentoxifylline (a drug that has
properties that include an influence on chemical
and cellular mediators of inflammation)
Figure 4
Herpetiform aphthous ulcers are present over
the anterior ventral tongue surface.
The
ulcerations are small, clustered and tender,
but are not preceded by a vesicular phase.
Table 2 - Aphthous Ulcers vs. Secondary Herpes Simplex Infection
Aphthous Ulcers
Herpes Simplex
Etiology
Immune dysfunction
HSV1
Triggers
Stress, trauma, diet, hormones,
depressed immunity
Stress, trauma, ultraviolet light,
depressed immunity
Prodrome
Little prodrome
Prodromal symptoms
Appearance
Nonspecific microscopy, no
vesicles, single, oval ulceration
Viral cytopathic changes, vesicles pre-
cede ulcers, multiple, confulent ulcers
Sites
Nonkeratinized mucosa
Keratinized mucosa
Treatment
Corticosteroids, topical tetracycline
rinses
Antiviral treatment