Quality Resource Guide –
Oral Ulcerative and Vesiculobullous Diseases Part 1 - 4th Edition
www.metdental.com
Page 2
Table 1 - Clinical Features of Aphthous Ulcerations
Minor Aphthae
Major Aphthae
Herpetiform Aphthae
Size
<0.5 cm
>1.0 cm
<0.5 cm
Shape
Oval
Ragged, oval, crateriform
Oval
Number
1-5
Usually solitary
10-100
Location
Nonkeratinized mucosa
Nonkeratinized mucosa
Any intraoral site
Treatment
Topical corticosteroids,
tetracycline mouthrinse,
immunosuppressives,
topical anesthetics
(lidocaine, benzocaine)
Topical/systemic/intra
lesional, corticosteroids,
thalidomide
Topical/systemic
corticosteroids,
tetracycline mouthrinse
Deficiencies of vitamin B12, folic acid, and iron
as measured in serum have been found in only a
small percentage of patients with aphthous ulcers.
Correction of these deficiencies has produced
improvement or cures in this small group. Patients
with malabsorption conditions such as celiac
disease and Crohn’s disease may also develop
aphthous-type oral ulcers.
Other causes or alternate etiologies of aphthous
ulcers that have been investigated include family
history, hormonal alterations, stress, trauma, and
food hypersensitivity including nuts, chocolate, and
gluten, among others, though only anecdotally,
such as tomatoes and spicy foods. None of these
is seriously regarded as being important in the
primary causation of aphthous ulcers, although
any of them may have a modifying or triggering
role. Although HIV-positive patients may have
more severe and protracted aphthous-like ulcers,
the role of HIV and other agents is unknown.
The degree of immunosuppression appears to
be more related to the major form of aphthous
ulceration as measured by both peripheral blood
CD4+ T-cell subsets and neutrophils within this
population. More recently,
it has been proposed
that gamma/delta - T-lymphocytes may have a role
in an antibody-dependent cell-mediated cytotoxicity
reaction toward oral epithelium. Systemic diseases
or conditions may also influence development
of or be associated with aphthous ulcers. These
include celiac disease, inflammatory bowel disease,
neutropenia and use of certain drugs such as
methotrexate. Of note is the recent hypothesis that
aphthous type ulcerations may be associated with
an autoinflammatory disease group of conditions
or periodic syndromes, including Behcet’s disease.
Clinical Features
Three forms of aphthous ulcers have been
recognized: minor, major, and herpetiform aphthous
ulcers (Table 1). All forms present as painful
recurrent ulcers that heal within 10 to 14 days.
Patients occasionally have prodromal symptoms
of tingling or burning before the appearance
of the lesions. Importantly, the ulcers are not
preceded by vesicles and characteristically appear
on the vestibular and buccal mucosa, tongue,
soft palate, fauces, and floor of the mouth (non-
keratinized sites). These lesions rarely occur on the
attached gingiva and hard palate, thus providing
an important clinical sign for the separation of
aphthous ulcers from secondary recurrent herpetic
ulcers. In the patient with AIDS or HIV disease,
however, aphthous-like ulcers may involve any
mucosal site.
Minor Aphthous Ulcers
Minor aphthous ulcers are the most commonly
encountered form of aphthous ulceration
(Figures 1, 2) and affect about 80% of those with
RAS. This type usually appears as a single to a
few painful, well defined oval or round ulcers, less
than 0.5 cm in diameter. They are covered by a
yellow fibrinous membrane and surrounded by
an erythematous halo. When the lateral or ventral
surfaces of the tongue are affected, pain tends to
be out of proportion to the size of the lesion. Minor
aphthous ulcers generally last 7 to 10 days and
heal without scar formation. Recurrence patterns
vary across patients; individuals may not have
clinical lesions for periods ranging from weeks to
years, while in others, recurrences on a regular and
frequent basis are the rule.
Major Aphthous Ulcers
This form of aphthous ulceration is regarded
as the most severe expression of aphthous
stomatitis (Figure 3), affecting about 10% of
those with aphthous ulcers. Lesions are larger
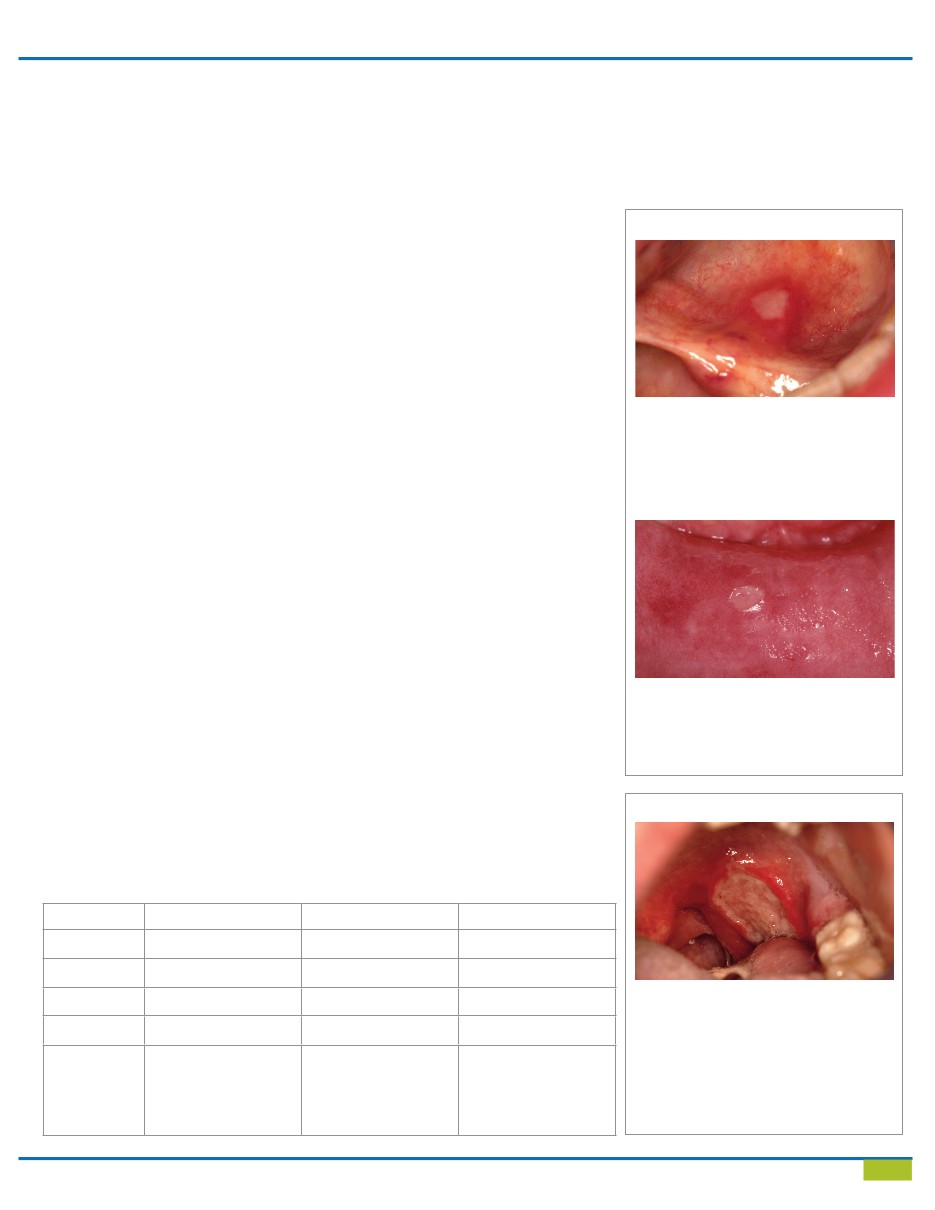
A small, solitary minor aphthous ulcer involving
the lower labial mucosa demonstrates a yellow-
ish fibrinous base with a well defined periphery.
This is representative of a later, less symptomatic
phase of the condition as healing progresses.
Figure 2
A slightly irregularly marginated aphthous
ulceration over the anterior floor of the mouth
with a characteristic fibrinous base located and
a brisk peripheral inflammatory reaction as
representative of an early acute phase lesion.
Figure 1
Figure 3
This major aphthous ulcer of several weeks
duration measures over 2 cm in diameter with
a cratered periphery and fibrinous surface. A
thin circumferential inflammatory rim is pres-
ent. Management strategies may include those
aimed at transitory symptomatic relief with
topical anesthetics, topical, systemic and intra-
lesional steroids, and in severe or recalcitrant
cases, thalidomide may be considered.