Page 6
Quality Resource Guide –
Xerostomia Revisited 4th Edition
www.metdental.com
One approach to restoring salivary gland function
may entail the use of sialagogue or secretagogue
medications that stimulate secretions from the
glands. These agents are classified as cholinergic
agonists (Table 4). Their efficacy, however, is
limited to patients whose salivary glands have
functional secretory components. Since these
drugs require systemic administration in order
to stimulate the cholinergic receptors of the
salivary glands, they can also cause a variety of
uncomfortable or intolerable side effects. These
include flushing and sweating. At higher doses
they can cause urinary frequency, abdominal
cramping, and diarrhea. These salivary stimulents
are contraindicated in patients with asthma,
glaucoma, and cardiac arrhythmias.
For the management of the unpleasant symptoms
of xerostomia and to contribute to a sensation of
oral moistness, a number of products have been
developed that are designed to replace saliva and
also provide ingredients that simulate those in
natural saliva (Table 4). They are available over-
the- counter, but their duration of efficacy may
be brief, and frequent re-administration may not
be cost effective. These products are available
as oral solutions, aerosols, sprays, gels, or
mouth swabs. Sugarless chewing gum may also
aid in keeping the mouth moist by stimulating
some natural salivary flow. Agents that contain
glycerin may be effective by contributing to a
sensation of increased moistness by increasing
oral lubrication (Table 4). An extensive systematic
review of multiple studies that have evaluated
the comparable efficacy of various xerostomic
therapies found no evidence that any of the
currently available remedies was particularly
effective. In this regard it should be noted
that it is difficult to accurately assess the
therapeutic efficacy of any intervention because
of the inherent variation in salivary function
between patients and the wide range of highly
subjective perceptions of patients’ xerostomic
symptoms. As noted in the introduction of this
Guide, there also appears to be little correlation
between patient symptoms and the degree of
hyposalivation. Long-term and costly placebo-
controlled clinical trials would be required to
determine whether or not saliva replacement
therapies are effective in preventing or reducing
the symptoms of xerostomia.
Furthermore,
evidence-based outcomes of such studies would
not ensure that a product is more effective if
based solely on patient assessment.
A non-foaming (non-detergent) dentifrice
that does not contain sodium lauryl sulfate is
recommended for xerostomic patients, since
this ingredient, contained in most dentifrices,
can have a deleterious effect on the protective
mucin layer of the oral mucosa that is already
compromised in these patients.
Other palliative strategies include frequent
sipping of water or holding ice chips in the
mouth. Use of a humidifier, particularly at night,
may offset the reduced amount of saliva that is
produced during sleep, and may be particularly
beneficial for mouth breathers.
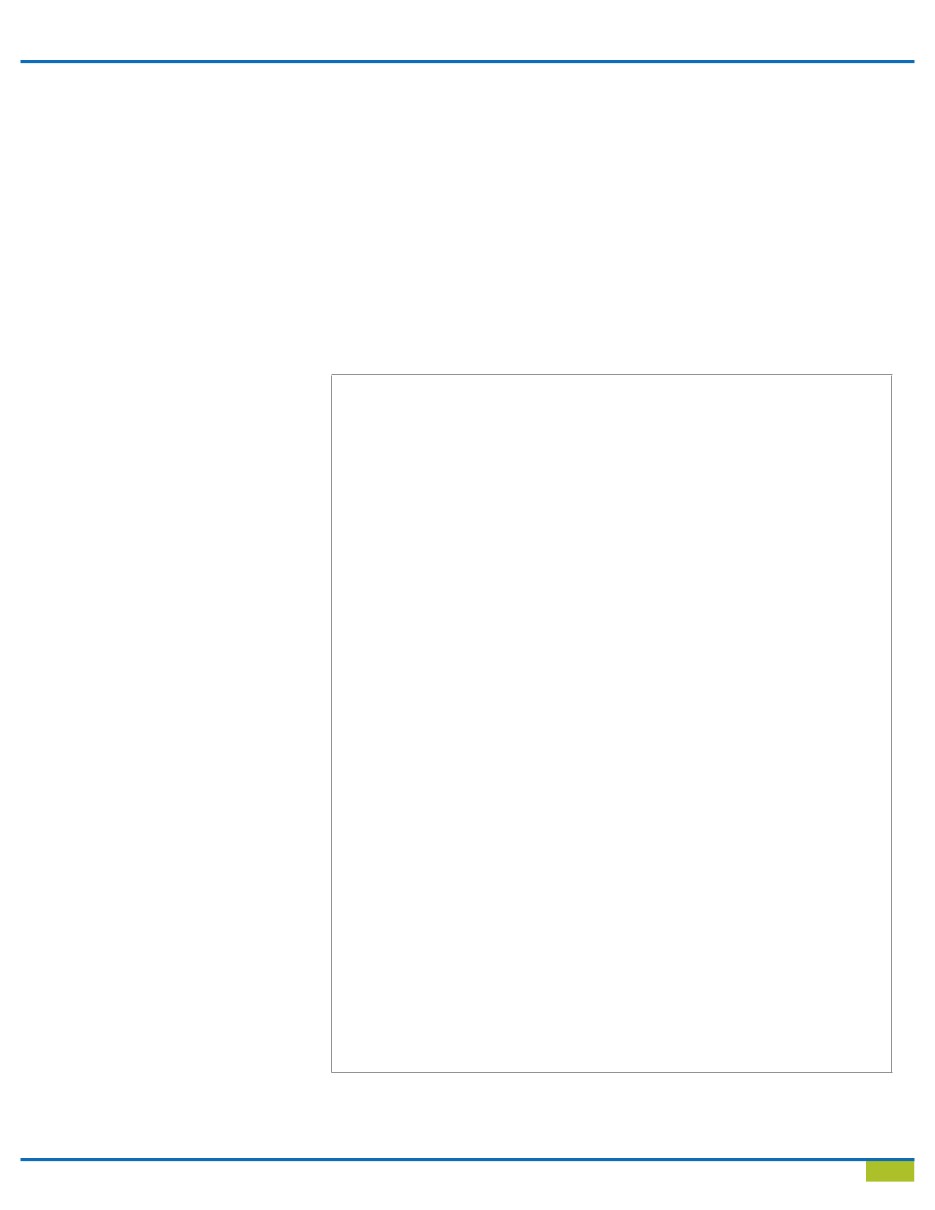
Table 4 - Therapeutic Options for Xerostomic Patients*
Pharmacologic Salivary Stimulants
Pilocarpine (Salagen®)
Cevimeline (Evoxac®)
Examples of Saliva Substitutes
Biotene® Oral Balance® products
Moi-Stir® products
MouthKote®
Optimoist®
Salivart®
Oasis® moisturizing mouth wash
(contains glycerin)
Tom’s of Maine® natural anticavity fluoride mouthwash for a dry mouth (contains glycerin)
Examples of Fluoride Supplements Over-the-counter
Gel-Kam® gel
ACT®, Fluorigard® rinse
Prescription
Fluoritab® drops
Thera-Flur® drops
Karigel® gel
PreviDent® dentifrice or gel
Fluorinse® rinse
Lozi-tab® chewable tablet
Karidium® chewable tablet
Duraflor® varnish
Electrostimulation devices
Candidal Infections
Mycostatin® oral suspension
Mycostatin® pastilles
Mycelex® troche
*
Source:
Wynn RL, Meiller TF, Crossley HL. 2007-2008 Drug Information Handbook for Dentistry. 13th ed.
Hudson, OH: Lexi-Comp; 2007; pp 1812-1820.