Page 3
Quality Resource Guide –
Xerostomia Revisited 4th Edition
www.metdental.com
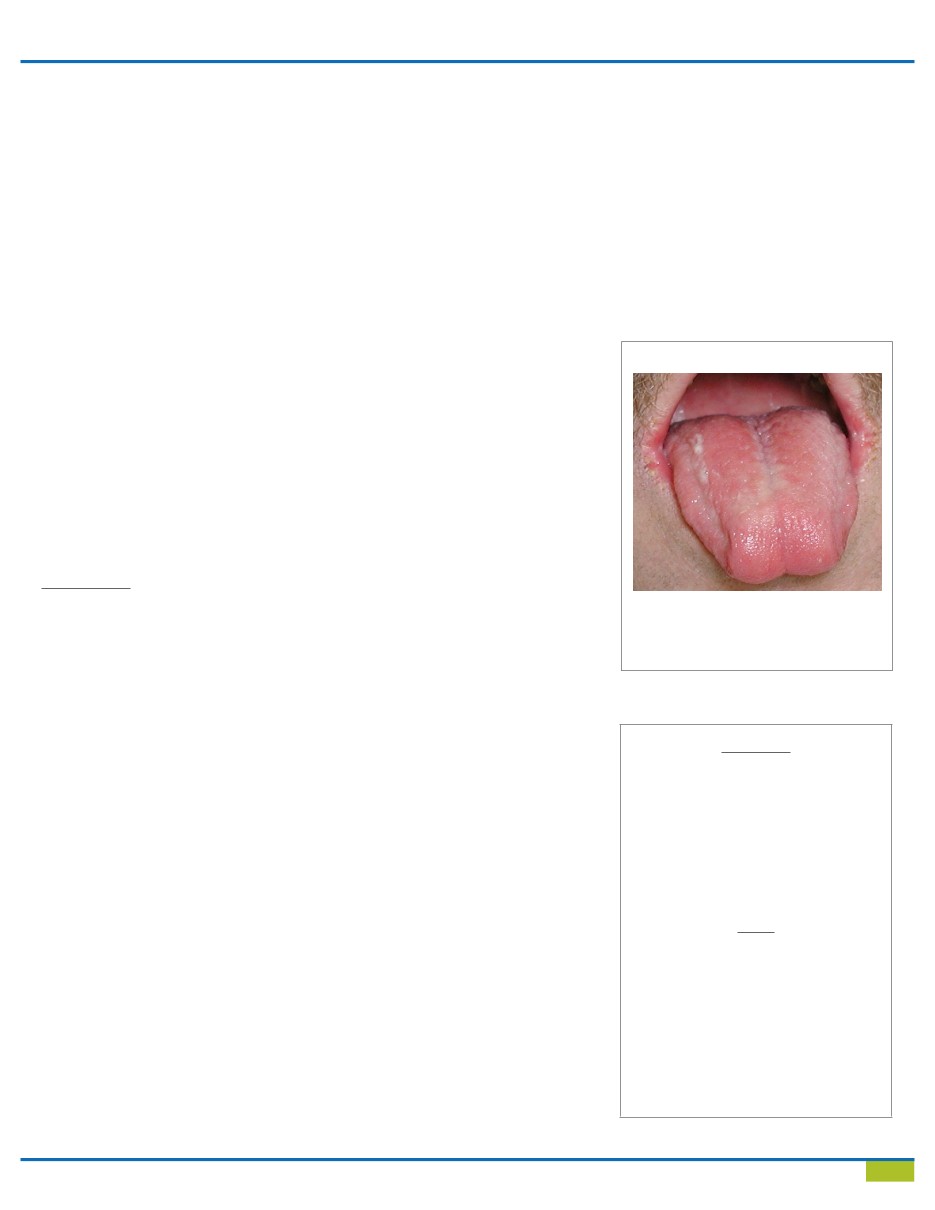
The patient with xerostomia may develop a variety
of oral manifestations (Table 3). One common sign
is erythema of the tongue, with loss of papillae and
increased fissuring (Figure 1). The oral mucous
membranes may appear parched, and rubbing a
finger or mouth mirror over their surfaces may
result in their sticking to rather than sliding over
the tissues. The saliva may appear “frothy” or
“stringy” (Figure 1), and it may not be possible to
elicit secretions from the parotid or submandibular
gland ducts.
secondary Sjögren’s syndrome, a disease that
causes a progressive destruction of the secretory
components of the salivary glands. The similar
but less common “primary” Sjögren’s syndrome
usually develops in women over 50 years of age
(post menopause) who may also have rheumatoid
arthritis in association with dry eyes secondary
to loss of tear gland function. Xerostomia is also
encountered in patients with diabetes mellitus,
HIV/AIDS, hepatitis C, and renal disease but in
these individuals the condition may, in part, be
a manifestation of the xerogenic effects of the
multiple medications that they are likely to be
taking.
Graft-versus-host disease develops in patients who
have undergone bone marrow transplantation and
has features similar to those of other autoimmune
disorders. The recent literature has added sleep
apnea and its treatment with continuous positive
airway pressure (CPAP) as another prevalent source
of xerostomia.
3.
Radiation
Radiation therapy by external beam or brachytherapy
(where the radiation source is implanted close to the
tumor) may be used as the primary or adjunctive
treatment modality of squamous cell carcinomas
in the oral cavity or other malignancies that involve
the oral cavity or structures in the head and neck
region. If the area to be irradiated encompasses
or is in proximity to the parotid salivary glands,
permanent damage to the glands can occur and
result in xerostomia. A previous Quality Resource
Guide titled,
Management of the Oral Complications
Associated with Cancer Therapy
by Michaell Huber
has addressed the salient issues of xerostomia in
the patient with cancer of the oral cavity. In an effort
to reduce the risk of xerostomic complications,
radiation oncologists are actively engaged in
developing and testing a number of methods that
may be able to protect or at least limit the degree of
damage to the major salivary glands.
Another source of radiation exposure is from
radioactive iodine (I-131) that is used to treat thyroid
cancer. Cancers of the thyroid gland comprise
approximately 4% of all malignancies in women and
appear to be increasing in women ages 55 to 64.
Radioactive iodine has an affinity for accumulating
in the parotid glands. As a result, some of these
patients can develop a significant degree of
xerostomia which may be permanent.
Scientists at the National Institute of Dental Research
have been developing methods that eventually could
be used to restore or regenerate damaged salivary
glands using gene transfer technology that has been
successful in a number of medical applications.
Recognition
S
tudies have shown that the sensation
of dry mouth or a lack
of
saliva
may
not be perceived until salivary
flow has been reduced by as much as 50%.
This, however, can be influenced by the amount
that is normally produced which is subject to
considerable variation between patients. Patients
may describe symptoms that include a feeling of
oral dryness, burning sensations in the mouth,
lack of saliva or dryness while eating dry foods
in particular, or difficulty with swallowing (Table
3). Patients may also report a need to sip or
drink liquids while eating. Since less saliva is
normally produced at night, awakening at night
and experiencing a dry mouth may be another
manifestation. Patients may also complain of a
loss of or altered taste, problems with speaking,
and/or soreness or difficulty with retention of
dentures. A perception of malodour (bad breath)
has also been described. An affirmative response
to at least one of the following questions has
been shown to be a reliable indicator of a
reduction in saliva: (Fox criteria)
2
• Does your mouth usually feel dry?
• Does your mouth feel dry while eating a meal?
• Do you have difficulties swallowing (dry) foods?
• Do you sip liquids to aid in swallowing?
• Is the amount of saliva in your mouth too little
most of the time or don’t you notice it?
An international study of 1,500 older patients found
that one question: “How often does your mouth feel
dry? Never? Occasionally? Frequently? Always?”
was equally reliable for determining the absence or
presence of xerostomia when the patient responses
were “never” or “always.”
Table 3 - Manifestations of Xerostomia
SYMPTOMS
Complaint of dry mouth
Increased need to keep mouth moist
Difficulty with eating, swallowing or speaking
Dry mouth during the night
Loss of taste
Sensations of burning, tingling or soreness
Bad breath
SIGNS
Loss of lingual papillae, fissured tongue
Frothy, stringy saliva
Erythema of the oral mucosa
Accumulation of plaque
Gingivitis, bleeding
Evidence of candidiasis
Cervical decalcifications
Cervical caries
Figure 1
This xerostomic patient exhibits an inflamed
and fissured tongue with atrophy of the fili-
form papillae and frothy saliva. There is also
angular cheilitis secondary to candidiasis.