|
Acute Gingival Conditions
Gingivitis
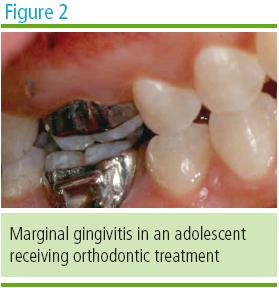
The development and rate of progression of gingivitis have been shown to be
age-dependent based on factors such as sex hormone changes that affect
host-parasite interactions, increased blood vessel permeability, exaggerated
responses to microorganisms, and lack of attention to proper oral hygiene
(Figure 2). Primary preventive strategies should be initiated to intercept
the process of reversible adolescent periodontal diseases; thereby, avoiding
the necessity to treat irreversible periodontal diseases in adulthood.
Necrotizing Ulcerative Gingivitis
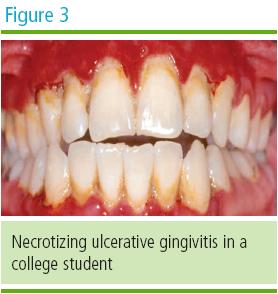
Necrotizing ulcerative gingivitis first appears most frequently during the
circumpubertal years. A stress-related component and an altered
host-resistance are associated with this condition (Figure 3). Causative
bacteria include Borelia vincentii and Prevotella intermedia. Clinically,
interproximal gingival necrosis is accompanied by rapid onset of gingival
pain. Treatment includes professional debridement of local irritants with
prophylaxis and scaling accompanied by meticulous personal home care using a
soft-bristled toothbrush. Therapeutic mouthrinses such as 0.2% chlorhexidine
gluconate solution can be recommended and in the presence of systemic
conditions, e.g. fever and adenopathy, antibiotics such as penicillin or
metronidazole can be prescribed. The presence of oral malodor associated
with necrotizing ulcerative gingivitis is yet another opportunity for the
dental team to promote a comprehensive oral health home care regimen.
Herpes Simplex
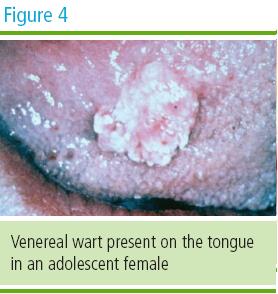
Adolescents who have not been exposed to the herpes simplex virus (HSV) can
be affected with a primary infection. Teenagers who engage in oral sex may
present with soft tissue lesions related to sexually transmitted diseases
and HSV-2 lesions in the oral cavity and perioral regions (Figure 4).
Questions related to the adolescent patientís sexual activity are advisable
in the presence of HSV lesions. While there is no known cure for HSV,
treatment for this condition is palliative. Antiviral medications such as
acyclovir along with analgesics such as acetaminophen can be prescribed to
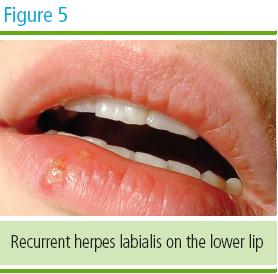
alleviate symptoms for the adolescent patient. Recurrent episodes of herpes
labialis (RHL) may be treated with pencyclovir cream for perioral lesions
(Figure 5).
Third Molars
The extraction of impacted third molars is an anticipated event by many
adolescents. Third molars usually emerge between the ages of 17 and 25
years. During the process of eruption, the development of pericoronitis is a
common, pain-causing sequela. Periodontal therapy in this region should
focus on eliminating pathogenic bacteria.
Periodontal
disease around asymptomatic third molars may progress even in the absence of
symptoms. This should prompt dentists to monitor the eruption of third
molars in adolescent patients. Periodontal disease is indicated by probing
depths > 4 mm around these teeth. Further anaerobic bacterial infection may
spread from the supporting tissues surrounding the third molars to other
teeth, particularly the second molars. This may result in the disruption of
the periodontal ligament, root resorption, and pocket depth associated with
loss of attachment. These factors should alert the dentist to thoroughly
evaluate the third molars in adolescent patients to identify and prevent the
onset of periodontal disease.10 Despite local lavage and the administration
of systemic antibiotics and analgesics, if the periodontal pockets and/or
symptoms persist extraction of the third molars may be the most prudent
long-term solution.
Another
consideration is the evaluation of third molars in adolescent female
patients who are pregnant. Periodontal pocketing around third molars has
been linked to a higher incidence of premature births. Not only should
dentists evaluate periodontal pockets surrounding the third molars of their
pregnant female adolescent patients, but all women of childbearing age for
systemic risks from oral inflammation associated with periodontal
pathology.11 In addition, research suggests that women of childbearing age
who take oral contraceptives may have a higher incidence of post-third molar
extraction dry socket (localized osteitis).12 For further information on
womenís oral health, the reader is referred to the MetLife Quality Resource
Guide entitled Womenís Oral Health Concerns, 2nd Edition.
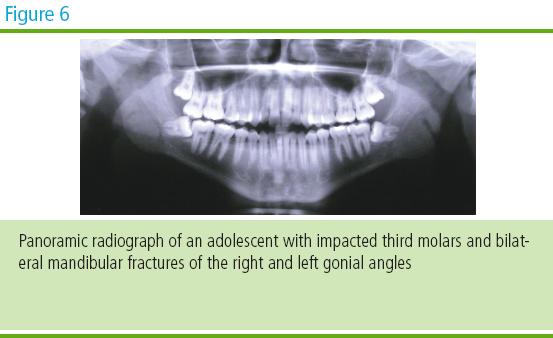
Impacted third
molars may pose an additional concern. For example, the presence of impacted
third molars or their extraction make the gonial angle of the mandible more
susceptible to fracture in adolescent athletes (Figure 6).
|